In recent years, the advancement of materials used in the dental and medical fields has significantly improved the quality of care and treatment options available to patients. Among these materials, zirconia (zirconium dioxide) has emerged as a popular choice for dental restorations, including crowns, bridges, and implants, due to its exceptional durability, aesthetic qualities, and biocompatibility. However, zirconia allergy, zirconia crown allergy in particular, has made it to the spotlight in recent years, as with the increased use of any biomaterial, there comes a concern for potential adverse reactions, including allergies. Although relatively rare, allergies to dental materials, including zirconia, are a topic of growing interest and concern among dental professionals and patients alike.
Allergic reactions to dental materials can manifest in various ways and potentially compromise the success of dental implants or restoration. Given zirconia’s prevalence in modern dentistry, understanding the nature of zirconia allergies, their symptoms, diagnosis, and management becomes essential.
This article aims to shed light some light on this allergy, focusing on specific areas such as zirconia crown and implant allergies and the broader category of zirconium oxide allergy. By delving into clinical findings, expert opinions, and patient experiences, we aim to provide a comprehensive overview that can guide both dental professionals’ and patients’ decisions regarding dental treatments.
Understanding Zirconia
Zirconia, or zirconium dioxide, is a ceramic material that has gained widespread acclaim in the dental industry for its remarkable properties. Known for its exceptional strength and durability, zirconia closely mimics the appearance of natural teeth, making it an ideal choice for various dental applications. Its use spans from crowns and bridges to dental implants, offering patients a blend of aesthetic appeal and long-lasting functionality.
The material’s biocompatibility is a key feature contributing to its popularity. Its inert nature means it interacts well with the human body, posing minimal irritation or adverse reaction risk when used in dental restorations. This compatibility makes it a preferred option for patients seeking reliable and safe dental solutions.
Comparison with Other Dental Materials
Zirconia stands out among other materials traditionally used in dentistry, such as metal alloys and porcelain.
Metal alloys, while strong, often lack the natural appearance that zirconia can provide and may cause allergic reactions in some patients due to nickel or other metals.
Porcelain, another popular choice, offers excellent aesthetic results but does not match the strength and resistance to wear that zirconia boasts.
The superior mechanical properties of zirconia include its high fracture toughness and resistance to wear, making dental restorations crafted from this material highly durable and capable of withstanding the daily forces of chewing and biting. Additionally, zirconia’s ability to be color-matched to the surrounding teeth ensures that restorations perform well and seamlessly blend with the natural dentition, enhancing the overall appearance of the patient’s smile.
Zirconia Crown Allergy
Despite zirconia’s widespread adoption and benefits in dental restorations, patients have reported allergic reactions to zirconia crowns. Though relatively rare, these reactions question the sensitivity some individuals may have to dental materials made from them.
Symptoms Associated with Allergic Reactions to Zirconia Crowns
Patients who have experienced allergic reactions to zirconia crowns report a variety of symptoms, which can include but are not limited to:
- Inflammation of the gums or soft tissues surrounding the crown
- Redness and swelling at the site of the crown
- Itching or discomfort in the affected area
- Less commonly, systemic symptoms such as dermatitis or rashes elsewhere on the body
These symptoms can emerge shortly after the placement of a zirconia crown or may develop over time, complicating the diagnosis and often leading to confusion with other dental issues such as infection or improper crown fit.
Diagnostic Challenges and Methods
Diagnosing an allergy to zirconia crowns presents several challenges. There is no standardized test (at least at the time of writing this article) specifically for the material’s sensitivity, which means that dentists and allergists often have to rule out other potential causes of the symptoms. This process can involve:
- Reviewing the patient’s dental and medical history for other allergies or sensitivities
- Conducting patch tests with various materials, including metals that are common allergens, to identify potential cross-reactivities
- Removing the crown temporarily to observe if symptoms improve can serve as an indirect indication of material sensitivity.
In cases where zirconia crown allergy is suspected, collaboration between dental professionals and allergists is crucial for accurately diagnosing and managing the condition.
Research and clinical reports on zirconia crown allergies are limited, reflecting the rarity of such reactions. However, the documented cases emphasize the importance of awareness and vigilance in monitoring patients’ responses to zirconia restorations. Dental professionals are encouraged to consider material sensitivity as a potential cause of unexplained symptoms surrounding dental restorations and to engage in open discussions with their patients about the materials used in their care.
Understanding this type of allergy is an evolving area of dental medicine. As the use of zirconia continues to grow, so too does the need for comprehensive research and reporting on adverse reactions to ensure that all patients receive care that is not only effective but also safe and tailored to their individual health needs.
Zirconium Oxide Allergy
Zirconium oxide, the primary component of zirconia used in dental and medical applications, is recognized for its excellent biocompatibility and low allergy risk. However, the possibility of an allergic reaction, albeit extremely rare, prompts a closer examination of zirconium oxide as a potential allergen.
Understanding Zirconium Oxide
Zirconium oxide is the base material for zirconia ceramics, renowned for their strength, durability, and compatibility with human tissues. Its widespread use in dentistry, especially for crowns and implants, is a testament to its safety and effectiveness. Despite this, the potential for allergies cannot be entirely dismissed, necessitating a deeper understanding of how these reactions could occur.
The rarity of Zirconium Oxide Allergies
Allergic reactions to zirconium oxide are notably rare, with very few documented cases in medical literature. This rarity is attributed to the material’s stability and inertness, which minimizes its potential to elicit an immune response. Unlike metals such as nickel, known allergens and present in some dental alloys, zirconium oxide does not typically release ions that could trigger allergies.
Expert Opinions and Research Studies
Expert opinions and research studies on zirconium oxide highlight its biocompatibility and low allergenic potential. Studies exploring the allergenic potential of dental materials, including zirconium oxide, are crucial for advancing our understanding and ensuring patient safety.
Researchers are exploring more about the immune system’s interactions with various dental materials, aiming to identify any conditions under which an allergic response to zirconium oxide could be provoked. These investigations are key to developing even safer materials and treatment options for dental care.
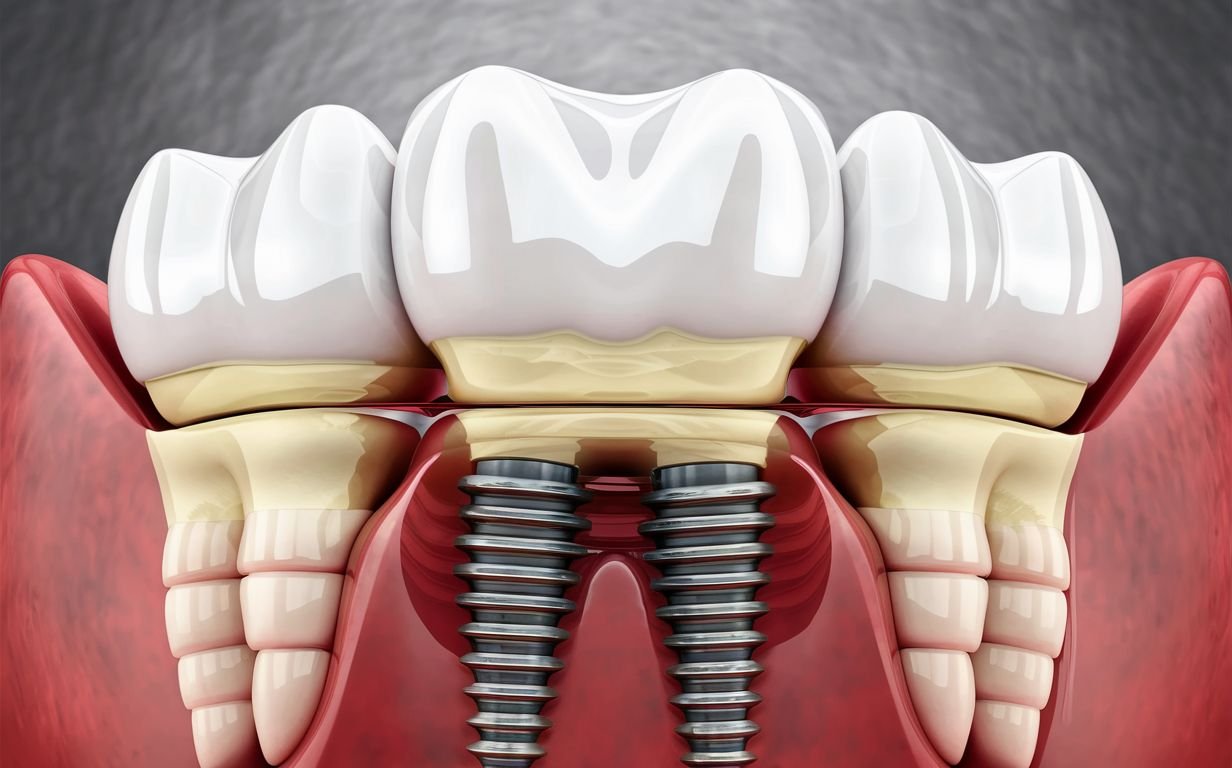
Zirconia Implant Allergy

The advent of zirconia implants has marked a significant milestone in dental prosthetics, offering a metal-free alternative to traditional titanium implants. This new implant material, praised for its aesthetic appeal and biocompatibility, has become a popular choice for patients seeking a holistic approach to dental care. However, the question of whether zirconia implants can provoke allergic reactions remains a point of consideration for dental professionals and patients alike.
Incidence of Allergic Reactions to Zirconia Dental Implants
Allergic reactions to zirconia dental implants are extremely rare, mirroring the low incidence of allergies to zirconium oxide itself. Zirconia’s chemical stability and lack of corrosion contribute to its suitability as an implant material, minimizing the risk of releasing allergenic particles into the surrounding tissues. Despite this, isolated cases of sensitivity or allergic reactions have been reported, underscoring the importance of vigilance and patient-specific considerations in dental care.
Symptoms and Diagnosis of Zirconia Implant Allergies
Symptoms indicative of a potential allergic reaction to a zirconia implant may include localized swelling, redness, or discomfort around the implant site, sometimes accompanied by systemic manifestations such as skin rashes. Diagnosing an allergy to a zirconia implant involves a comprehensive evaluation, including a detailed patient history, to rule out other causes of the symptoms, such as infection or mechanical irritation from the implant.
Given the scarcity of reported allergic reactions to zirconia, specific diagnostic tests for zirconia sensitivity are not widely available. In cases where an allergy is suspected, consultation with an allergist and consideration of alternative materials may be necessary to ensure patient safety and comfort.
Patient Case Studies and Outcomes
The literature on zirconia implant allergies includes a handful of case studies, providing insights into the clinical presentation and management of such cases. Successful outcomes often involve the removal of the zirconia implant and replacement with an alternative material, resulting in the resolution of allergic symptoms. These case studies contribute valuable knowledge to the field, aiding dental professionals in identifying and addressing potential material sensitivities.
Diagnosis and Management of Zirconia Allergies
Diagnosing and managing allergies to zirconia, particularly in the context of dental implants, involves a comprehensive approach that considers the rarity of such reactions and the need for accurate identification to ensure patient safety and well-being.

Diagnosing Zirconia Allergies
Given the infrequency of zirconia allergies, diagnosing this condition poses a unique challenge for healthcare professionals. The process often involves a combination of patient history, clinical examination, and exclusion of other potential causes of symptoms. Key steps in the diagnostic process include:
- Patient History: A detailed medical and dental history can provide clues about a patient’s propensity for allergic reactions. Information about previous reactions to dental materials, jewelry, or other metal exposures can be particularly telling.
- Clinical Examination: Physical signs of allergy, such as localized inflammation, redness, or rash around the implant site, warrant further investigation. However, these symptoms can also indicate infection or other non-allergic responses.
- Patch Testing: Although specific tests for zirconia sensitivity are not standard, patch testing with various dental materials can help identify or rule out common allergens. This method, however, has limitations and may not definitively confirm a zirconia allergy.
- Implant Removal: In cases where an allergy is strongly suspected and other causes have been excluded, removing the zirconia implant may be considered to observe if symptoms resolve. This approach is typically a last resort due to the invasive nature of implant removal and replacement.
Management of Zirconia Allergies
For individuals diagnosed with a zirconia allergy, management strategies focus on alleviating symptoms and preventing future reactions. Options include:
- Alternative Materials: Choosing alternative materials for dental restorations or implants is a primary consideration. Materials such as titanium, which has a long history of successful use and low allergenic potential, may be recommended.
- Symptom Management: For minor reactions, topical or systemic corticosteroids may be prescribed to reduce inflammation and discomfort. Antihistamines can also be effective in managing mild allergic symptoms.
- Long-term Monitoring: Patients with a history of zirconia allergy should be closely monitored in future dental treatments. Informing dental care providers of the allergy is crucial to avoiding using zirconia in future restorations or prosthetics.
- Patient Education: Educating patients about their allergies and potential material alternatives empowers them to make informed decisions about their dental care and to advocate for their health in clinical settings.
The management of zirconia allergies underscores the importance of personalized care in dentistry. By taking a patient-centered approach, dental professionals can ensure that treatments achieve aesthetic and functional goals and maintain the highest standards of patient health and safety.
Alternatives to Zirconia in Dental Applications
The dental industry offers several viable options for patients who have experienced allergies to zirconia or are seeking alternative materials for dental restorations due to personal preferences or health concerns. Each alternative has advantages and considerations, enabling tailored treatment plans that align with individual needs and circumstances.
1. Titanium:
- Pros: Titanium is renowned for its exceptional strength, biocompatibility, and corrosion resistance. It has a long history of successful use in dental implants and is generally well-tolerated by the body, with a very low risk of allergic reactions.
- Cons: Titanium is a metal; although rare, some individuals may have or develop allergies to metals. Aesthetically, titanium may only sometimes match the natural color of surrounding teeth as closely as zirconia.
2. Porcelain Fused to Metal (PFM):
- Pros: PFM crowns balance strength (from the metal) and aesthetics (from the porcelain overlay). They have been a staple in restorative dentistry for decades.
- Cons: The metal underlying the porcelain can sometimes create a grayish tint at the gum line. Additionally, there is a small risk of metal allergies.
3. All-Porcelain or All-Ceramic:
- Pros: These materials provide excellent aesthetic results, matching teeth’ natural translucency and color. They are also biocompatible and suitable for individuals with metal sensitivities.
- Cons: While modern ceramics are much stronger than in the past, they may still be less durable than zirconia or metal-based restorations, especially in areas of high bite pressure.
4. Composite Resin:
- Pros: Composite resins can be closely matched to the natural tooth color, are less expensive than other restorative materials, and are easy to repair.
- Cons: Resins wear down faster than ceramic or metal restorations and may stain over time, requiring more frequent replacement.
5. Gold Alloys:
- Pros: Gold alloys are durable, biocompatible, and offer a high degree of malleability, making them gentle on opposing teeth during chewing. They are suitable for patients looking for long-lasting restorations.
- Cons: The most obvious drawback is the color, which is not tooth-like, and the higher cost compared to other materials.
Why You Should Consider Alternatives:
Choosing an alternative to zirconia for dental restorations should be made in consultation with a dental professional, taking into account the patient’s medical history, aesthetic preferences, and functional requirements. Alternatives can provide safe and effective solutions for individuals with zirconia allergies without compromising health. Moreover, advances in dental materials continue to expand the options available, offering promising prospects for personalized and allergen-free dental care.
In conclusion, while zirconia stands out for its strength and aesthetic qualities, the dental field’s diverse array of materials ensures suitable alternatives for everyone. Through careful consideration and professional guidance, patients can achieve optimal dental health and satisfaction with their restorative outcomes.
Conclusion
Navigating the landscape of dental materials, particularly when considering allergies to widely used substances like zirconia, underscores the importance of personalized dental care. Although zirconia allergies are relatively rare, the potential for adverse reactions exists and warrants careful consideration by dental professionals and patients. The exploration of zirconia’s role in dental applications, alongside its allergenic potential, highlights the critical balance between leveraging advanced materials for their superior properties and ensuring they do not compromise patient health.
For those affected by or concerned about zirconia allergies, the dental industry offers a variety of alternative materials. From titanium and porcelain to composite resins and gold alloys, each option presents benefits tailored to meet different needs, preferences, and health considerations. A comprehensive evaluation should inform the decision to choose alternatives to an individual’s dental and medical history facilitated by open communication with dental care providers.
The evolution of materials science in dentistry continues to advance, promising the development of even more sophisticated, biocompatible, and hypoallergenic materials. This progress and a deeper understanding of material-related allergies pave the way for safer, more effective dental treatments. As we move forward, the emphasis on personalized care, informed choice, and patient safety remains paramount, ensuring that dental advancements serve the best interests of all patients.
In conclusion, while zirconia remains a cornerstone of modern dentistry for many good reasons, acknowledging and addressing the concerns related to zirconia allergies is crucial. By doing so, the dental community can continue to provide care that enhances oral health and aesthetics and upholds the highest standards of patient safety and well-being.